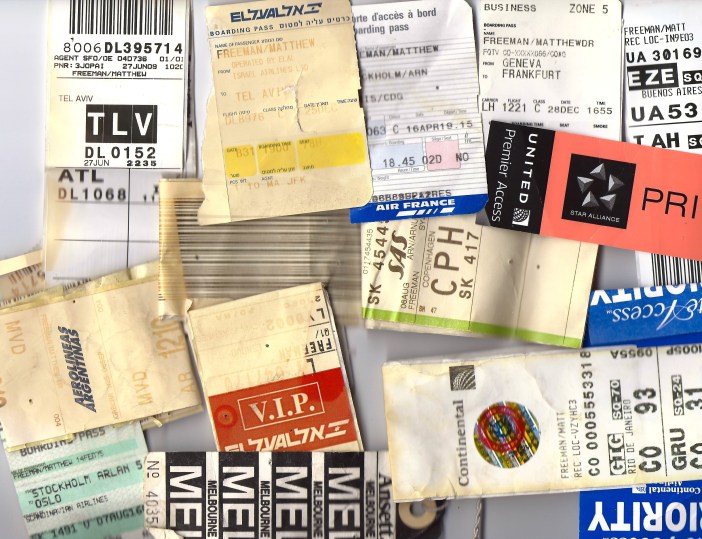
Matt Freeman
2 February 2018
The former patients discussed in this article are real; their names are pseudonyms.
Robert shifted in his chair. His blood pressure was a bit higher than normal, his complexion ruddy, and his eyes were somewhat bloodshot. I had already seen his blood work. Two of his liver enzymes were above normal, the average size of his red blood cells was higher than what one might expect. It was hardly a diagnostic conundrum. The 52-year-old man in my office was almost certainly an alcoholic.
I followed a careful, nonthreatening path in our conversation. I asked about sleep, stress, depression, and finally alcohol. He evaded the topic by saying he was a “social drinker.”
In a somewhat sneaky but effective maneuver, I examined his liver. As I let my hand slip beneath his right lower ribs, I asked, “Do you find yourself drinking more than you should?” It was as if he thought I could feel the bottle caps and wine corks in his abdomen. “Yes,” he replied. “I mean a lot.”
Once he was off the exam table and we could talk face to face, Robert assured me that he would never drink on duty. And he would never violate the 12-hour “bottle to throttle” rule. He is a captain, flying Airbus jets for one of the largest airlines in the world.
He had little difficulty “passing” his routine medical examinations to keep his license. He knew which medical examiners would ask the fewest questions, thereby ensuring that both the doctor and the pilot would maintain job security.

“So many of us drink.” Robert was sullen. “You’re alone in some hotel room. There is no way to unwind. It just becomes a habit. More than a habit.”
Robert is not alone.
Air travel and alcohol abuse have a longstanding partnership. Higher-risk drinking has been described as a “silent epidemic” among passengers and crew alike.
The liquor culture of air transportation is due in part to economics.
During the 1970s, airfares on US airlines were regulated by the Civil Aeronautics Board. Since the airlines could not compete on price, they competed with service. Alcohol was often cornerstone of competition. Jumbo jets were fitted with bars in both economy and first classes, Delta Air Lines began offering complimentary champagne, and National Airlines offered complimentary alcohol of any kind. Eastern Air Lines described complimentary alcohol as “unconscionable,” but market forces drove them to offer free booze as well.
American Airlines pioneered the Bloody Mary. Viewed as a socially acceptable cocktail for the morning, passengers consumed the vodka-laced tomato juice with zeal. American reportedly turned the bottlers of Mr. and Mrs. T. Bloody Mary Mix into millionaires.

Mechanics at American noticed that some of their planes were sustaining daily gouges to their cabin walls. The source of the damage turned out to be from bar carts jamming into the wall. The crew were serving liquor so early during a flight’s ascent that they could only stop the carts effectively by letting them jam into the wall.
In 1972, Southwest Airlines engaged in an airfare war with a competitor. Passengers were offered the opportunity to purchase a ticket for $13 or pay $26 for the plane ticket and receive a bottle Chivas Regal scotch whiskey. More than three quarters of the passengers chose to pay double and buy the bottle of whiskey as well as the plane ticket, making Southwest the largest distributor of Chivas in Texas.

In the post-deregulation era, alcohol continued to serve as a selling point. Airlines compete by offering complimentary liquor. In business and first classes, air carriers feature sommeliers, who have selected finer wines for their higher-paying guests. On the ground, open bars welcome passengers in airline lounges. Industry consultants have noted that passengers will sometimes select an airline based on its liquor policy.
Forty-four years after its free Chivas offer, Southwest Airlines was still unabashed by its promotion of tipsy flying. Passengers on a three hour, twenty-minute flight from Oakland to Kansas City earned an announcement of congratulations from the captain. The passengers had emptied out all of the bar carts on the airplane.
The “high life” of champagne and Scotch whiskey above the clouds can often have a dark side.
Hugh, 52, travels for 40 weeks per year. As a salesperson, he dines out at least three nights per week. At sales dinners, he typically has a few glasses of wine followed by a few glasses of Scotch. That is three times the recommended alcohol intake from the Centers for Disease Control and Prevention (CDC) guidelines. When Hugh boards a flight to his next destination, he usually has a Scotch prior to takeoff, and wine, beer, or whiskey in flight based on the length of the flight.
Although he came to see me for a routine physical exam, Hugh conceded that he is unhappy with his life. He is frustrated by his weight, poor sleep, lost sex drive, and lack of emotional connection to his wife. Unlike Robert, Hugh was not ready to talk. He never returned to have his blood drawn. I suspect he will find a primary care provider who will ask fewer questions. Perhaps he will just forego seeing a doctor entirely.
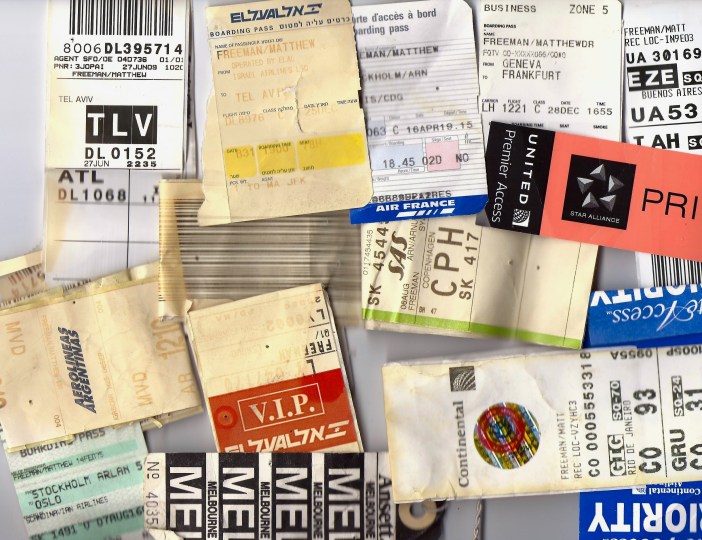
Frequent flyer like Hugh, the so-called “mobile elite,” can be predisposed to problematic drinking. Studies of the frequent flyers have yielded a profile of passengers who socially isolated. While flying around the country or the globe, passengers like Hugh may lack the opportunity to engage in collective activities, and they may have frayed friendships. Relationships can become unequal: the frequent traveler may be away so often that he or she cannot participate equally in household chores, child-rearing, etc. Despite higher incomes and access to healthcare, this population is not in good shape.
 In some respects, the airlines enable Hugh and travelers like him. Catherine, 41, pours Scotch for passengers like Hugh. Catherine has been a flight attendant since she was 21. With two decades of seniority, she often finds herself rostered for her favorite trips: business class to Frankfurt. I met Catherine after an accident that occurred while she was off duty. She fell on the steps outside her apartment. Her blood alcohol content was 0.18 percent when it was measured in the emergency department. (Loss of consciousness can start at 0.2 percent; death at 0.5 percent.)
In some respects, the airlines enable Hugh and travelers like him. Catherine, 41, pours Scotch for passengers like Hugh. Catherine has been a flight attendant since she was 21. With two decades of seniority, she often finds herself rostered for her favorite trips: business class to Frankfurt. I met Catherine after an accident that occurred while she was off duty. She fell on the steps outside her apartment. Her blood alcohol content was 0.18 percent when it was measured in the emergency department. (Loss of consciousness can start at 0.2 percent; death at 0.5 percent.)
Dodging questions about alcohol, Catherine laughed as she describes her recipe for “crew juice.” This is a nickname for a punch made of any variety of combinations of liquor pilfered from the bar cart. Binge drinking—with “crew juice” or another source—is part the routine.
Getting drunk is not just an accident; it is an expectation.
Tina, 50, a senior flight attendant, complained that her employer sometimes lodged its crews in the same hotels as its passengers. “We can’t get drunk at the hotel bar,” she complained. Getting drunk, as far as Tina was concerned, was part of the itinerary.
Amanda Pieva, a journalist and flight attendant, wrote of the silent epidemic of alcoholism among crews. “We drink to help ourselves sleep when work disrupts our body clocks, and we drink when we run into long lost friends on our travels. While social drinking is the norm in society as a whole, it is amplified in the airline industry.”
Pieva continues, “The industry creates many alcoholics, most of whom are functional.” Since alcoholism is so widespread, Pieva argues that it has been normalized, and therefore not a topic of discussion.

Although Catherine appeared to be in denial, her drinking habits were unexceptional in her environment. Data from airline pilot surveys have shown that crews do not necessarily have a greater prevalence of alcoholism than the general population, but they tend to over-estimate the number of drinks required to become intoxicated. There was no pattern related to the type of aircraft flown nor the number of years of experience.
Pieva wrote, “Every single pilot or flight attendant I’ve talked to about this with adamantly agrees that alcohol abuse is a silent epidemic among us.”
The consequences of the silent epidemic are both short- and long-term, affecting both crew and passengers.
- In 2016 security staff smelled alcohol on a United Airlines pilot at Glasgow. A blood test taken two hours after his removal from the flight showed blood alcohol content more than double the upper limit.
- In 2013, a Pakistani pilot was imprisoned in the UK. His blood alcohol content was more than three times the normal limit He confessed to drinking three-quarters of a bottle of whiskey prior to the flight.
- In 2002, two America West pilots were ordered to taxi back to the terminal. Both were convicted of drunk flying.
- Alcohol was implicated in two fatal accidents in the former Soviet Union in 2011 and 2012.
Intoxicated passengers can pose a danger to themselves and others. In at least one documented instance, a passenger died during an otherwise survivable aircraft evacuation. His blood alcohol content was 0.24 percent. He had not even unfastened his seatbelt. the passenger who died was only one fatality. His alcohol-induced incapacitation could have easily impeded the evacuation of other passengers and crew.
A BAC of 0.24 percent is the equivalent of about ten drinks in a 160-pound man. If that seems like a lot, one investigator was served 12 drinks during a 90-minute flight.
The rise in “air rage” incidents is multifactorial, but alcohol has been implicated in at least 45 percent of reported disruptive passenger incidents. These disruptions can range from quiet disregard for safety to diversion of a flight. Surveys of airline passengers found that those who stated that they intend to consume alcohol on board were twice as likely to agree to the statement, “I rarely or never wear a seatbelt.” In more extreme circumstances, intoxicated passengers have engaged in obscene behavior, destroyed aircraft equipment, and threatened the safety of passengers and crew.

Passenger misconduct is widely deemed to be under-reported. An estimated one in 140,000 passengers engage in some form of misconduct per year. Up to one in a million are reported to have been involved in serious misconduct. This appears to be statistically infrequent until one considers that 650 million passengers fly annually. That is 650 cases of severe misconduct per year, and a little fewer than half of those cases have an alcohol component. At minimum, that is just under two serious alcohol-related misconduct incidents per day.
The risk persists after landing. In 2006, a passenger boarded a flight already intoxicated. He then purchased and drank two Jack Daniels “minis” on board a flight from Phoenix to Albuquerque. After landing, he drove from the airport, killing five in a motor vehicle crash. He died some hours later with a blood alcohol content of 0.32 percent.
Travel has been described as “situational disinhibition.” Airline passengers might engage in behavior that would otherwise seem uncharacteristic.
Alcohol itself reduces inhibition, and the combined forces can mean that passenger are less guarded. Binge drinking can be the start of a cascade of health-compromising behavior.
Studies of international travelers found that 20 percent of international travelers engaged in casual sexual relations while abroad. This applied to all types of travelers (business, leisure, family). A study of Belgians working overseas found that 51 percent of male workers had extramarital sex with local women, 31 percent with a commercial sex worker, and only 25 percent of almost 2,000 men in the study reported using a condom.
Alcohol intensifies the risk. Women who binge drink are five times more likely to contract gonorrhea, and report more sexual partners than women who consume alcohol in moderation.
The combined disinhibition from alcohol and the air travel environment can catalyze violence.
Sara Nelson, president of the Association of Flight Attendants, cited a lack of cabin staff, dark quarters, and alcohol as factors that can lead passengers to commit sexual assault. Although the proclivity to commit such an offense might exist on the ground, the aircraft cabin or the hotel away from home can provide the environment and the opportunity.
Onboard assault cases are hard to track: some are reported to local police, some to the FBI. The FBI reported 40 investigations opened in 2015, 58 investigations during the first half of 2016. The FBI acknowledges that about 75 percent of assaults are unreported.
There is no single tracking mechanism for inflight assaults, and flight crews do not receive training in the management of these situations. The crew have the burden of reporting disruptive behavior, but there is no box to tick for sexual assault.
Furthermore, reporting can be abbreviated or lost on international flights, where foreign law enforcement officials are involved.
 Defunct Hooters Air: the ultimate combination of sexism, alcohol, and flying.
Defunct Hooters Air: the ultimate combination of sexism, alcohol, and flying.
Flight attendants who have been assaulted are often unwilling to report the crime, “They’re not going to stop the plane. And then everyone’s going to be mad at you; you’re not a team player, you’re difficult” stated former flight attendant and assault victim Lanelle Henderson.
Henderson and others described assaults not just by passengers but by other crew members. Stories of intoxicated pilots assaulting flight attendants are common but rarely reported.
Male crew are not exempt from harassment. A flight attendant for JetBlue described frequent unwanted comments about the “Mile High Club,” and being grabbed or touched inappropriately by male and female passengers.
Sara Nelson described the notion that passengers can feel “out of the public eye” and therefore somehow get away with abusive behavior that they would otherwise eschew. The disinhibiting effects of alcohol combined with an altered sense of self can lead to behavior that can range from indecorous to criminal
Nelson described a conversation overheard by a coworker:
“When can we get some drinks around here, honey?’” asked several male passengers. While the flight attendant was still in earshot, “You can probably get sued for calling someone ‘honey’ nowadays.”
Although one could argue that these passengers could be chauvinists without alcohol, one can assume that alcohol diminishes or silences their superegos. In a service industry in which “the customer is always right,” passengers under the influence may feel somehow more entitled to be verbally or sexually abusive.
There is little incentive from the air transportation industry to restrict alcohol sales and consumption. In fact, restriction can affect profits. Irish low-cost airline Ryanair requested that airports limit alcohol to two drinks per person, and that airports ban serving alcohol before 10:00 am. Another low-cost carrier, Jet2 of the UK, stopped alcohol on morning flights.

Passengers resented the restrictions, claiming that the airlines had ruined their holidays. As one passenger put it, “Unless you’re being rowdy there’s no need [for a crackdown.]”
Airports that were affected by Ryanair’s restrictions claimed that the air carrier was really just attempting to increase its own inflight liquor sales. Moreover, airports depend on alcohol-mediated disinhibition to boost retail and duty free sales.
The duty free shop also provides a method to circumvent airline restrictions. Airline companies are reportedly inconsistent in their enforcement of company policies banning the consumption of alcohol that is not served by the airline crew. Passengers can stop by the duty free shop, even purchasing small liquor “minis” and secret them in their hand baggage for inflight consumption.

On flights with complimentary liquor, or in first and business class, there can be outcry from passengers who feel entitled to maximize their intake. First class passengers on American Airlines began tracking whether or not they were offered the alcoholic drink of their choice before the airplane had pushed back from the gate. They scorned flights in which they were offered water or orange juice, even though the flight had not even taken off. American had to post reminders to its crews to offer passengers their own (usually alcoholic) choice of drinks.
Robert did well. The last time I saw him he had been sober for close to a year, he was taking antidepressants, seeing a therapist, and feeling much healthier. But what about his coworkers who have not sought care? What measures can be taken for passengers and crew members to mitigate the “silent epidemic?”
Given the profits from serving liquor, airline companies and airport owners are unlikely to engage in meaningful efforts to encourage responsible drinking. There are no simple answers to curtail the epidemic and its consequences. At least a few interventions could incite a larger social movement.
1. Educate
There are a wide variety of web sites and magazines devoted to leisure and business travel. These are often found in airport lounges, hotels, or delivered to the homes of some credit card recipients.
Articles about quantifying alcohol intake, understanding limits, and recognizing problematic or addictive behavior could be both interesting and useful to readers.
Print and internet media could also offer lists of resources, such as Alcoholics Anonymous, therapists and addiction specialists may wish to advertise, there could even be support from organizations such as Mothers Against Drunk Driving (MADD).
For crew members, a review of blood alcohol content, the risks in the air and on the ground, and skills for working with intoxicated passengers and crew should be a part of initial and recurrent training.
Likewise, the airlines and their unions should reinforce alcohol abuse as a public health issue over a disciplinary concern so that those affected may be more like to seek help.
2. Include Airports, Lounges, and Hotels in Interventions
Since alcohol served on the ground before, during, and after flights contributes to the epidemic, those serving alcohol should be educated on polite but effective techniques for intoxicated patrons, such as “Distract, Delay, Dilute, and Deny.”
3. Institute Bystander Training for Airline Crews
In response to Title IX lawsuits pertaining to sexual assault on college campuses, many colleges and universities have introduced “bystander training.” These brief courses encourage confidence to intervene. As Lanelle Henderson described above, there is a fear that one could be “not a team player” or “uncooperative.” Bystander Training efforts could embolden crew members to intervene with respect: a quiet reminder that a fellow crew member has had enough to drink already.
Bystander training can also help curtail sexual assault among crewmembers. A crew member who has undergone bystander training may feel more comfortable telling a colleague that it is unwise to go to a hotel room alone, particularly if one or both have been drinking. The goal is to make such interventions expected as part of a community rather than a shock of assertiveness.
As a culture of respectful intervention grows, crew members may become more adept at intervening with intoxicated passengers.
4. The relationship between travel, alcohol, and sexually-transmitted diseases warrants attention and education.
Passengers and crew members deserve to know their risks for sexually-transmitted infections, and they deserve opportunities to learn about how to be screened, and how to protect themselves. Airlines and unions as well as travel web sites and magazines should address the sexually-transmitted disease epidemic and offer recommendations for healthcare providers and clinics that offer screening and treatment.=
For travelers and crew members also deserve evaluation for pre-exposure prophylaxis for HIV (PrEP). Those who have frequent unprotected sex with multiple partners, especially while traveling, and particularly those with a history of one bacterial sexually-transmitted infection, should be assessed for eligibility to take PrEP. This is a safe and effective means of preventing the transmission of HIV.
Condoms should be sold at airport retail outlets, and they should be available in crew lounges.

Some airports offer on-site medical clinics. Whenever possible, these clinics should be able to offer sexually-transmitted disease screening and treatment, post-exposure prophylaxis (medication for those who may have been exposed to HIV), and levenogestrel (“Plan B,” an emergency contraceptive or “morning after pill.”)
5. Women traveling alone deserve the opportunity for additional guidance and support.
Although both men and women can be affected, women traveling alone face specific vulnerability. Special efforts should be made to encourage responsible drinking, and how to seek help if one feels threatened—even if the threat seems benign. Passengers can slip notes on napkins to flight attendants, write messages on their mobile devices and show them to crew members, or speak to another passenger if the crew are not available.
Women’s magazines and web sites should offer constructive tips and advice for drinking with caution and avoiding higher-risk situations that could lead to a sexually-transmitted infection or sexual assault.
6. Provide Help Nearby
Most airports have interfaith “chapels.” For frequent flyers struggling with alcohol abuse, it would be wise to offer Alcoholics Anonymous meetings in these spaces. Although the timing may not suit everyone, an AA meeting could provide a safe alternative to the airport bar or airline lounge.
Employees might be too ostensible as they are amid coworkers and in uniform. Alcoholics Anonymous could have chapters near airports, or near areas where there are large or multiple crew hotels.
Liquor is a part of life. It is a part of traveling. Drinking can often be fun. I will have a drink (sometimes two) on a plane. But the prevalence of high-risk drinking surrounding air travel is far too dangerous to keep silenced.

References
Centers for Disease Control and Prevention. Alcohol and Public Health. http://www.cdc.gov/alcohol. Retrieved 21 January 2018
Cohen S. and Gössling S. A darker side of hypermobility. Environment and Planning. 2015; 47, 8
Dickinson G. The truth about drunk pilots – does the profession have an alcohol problem? The Telegraph. 24 January 2018
Feldman J. For Flight Attendants, Sexual Assault Isn’t Just Common, It’s Almost a Given. The Huffington Post. 22 November 2017.
Girasek DC & Olsen CH. Airline passengers’ alcohol use and its safety implications. Journal of Travel Medicine. 2009; 16: 311- 316
Gollan D. Seinfeld Redux: Are American Airlines Flight Attendants Saying ‘No Drinks for You’ in First Class? Forbes. 14 January 2016.
Halliday J & Topham G. Air passengers react to alcohol crackdown: ‘Get as many in as you can.’ The Guardian. 25 August 2017.
Hitt A, Ireland DR, & Hoskisson R. Strategic Management: Competitiveness & Globalization. Boston. Cengage Learning. 2017.
Hutton H., McCaul M., Santora P, Erbelding E. The relationship between recent alcohol use and sexual behaviors. Alcohol Clin Exp Res. 2008; 32, 2008-2015.
Modell JG and Mountz JM. Drinking and flying – the problem of alcohol use by pilots. The New England Journal of Medicine. 1990; 323: 455461.
Petzinger T. Hard Landing. New York: Times Books. 1995.
Pieva, A. The Airline Industry’s Drinking Problem. News Limited. 2017
Plush H. Pilot ‘congratulates passengers’ for drinking all of the alcohol on board. The Telegraph. 12 December 2016.
Schwartz K. Recent Incidents Put a New Focus on Sexual Assault on Airplanes. The New York Times. 20 October 2006.
Vivancos R, Abubakar I, Hunter PR. Foreign travel, casual sex, and sexually transmitted infections: systematic review and meta-analysis. International Journal of Infectious Diseases. 2010;14(10):e842–51.
Ward B. Travel and sexually transmitted infections. Journal of Travel Medicine 2006; 10.
©2018
All images labelled for commercial reuse









 The taste was not entirely natural. Lemon, grapefruit, and orange were convincingly similar to the fruit found in nature. Watermelon, grape, and lime bore little resemblance to the actual fruit, but rather resembled the imaginary flavors found in soda and candy. The flavor, for example, was rich with the taste of lime. It was not at all like the lime that grows on trees; it was a perfect, rounded, floral taste of lime candy.
The taste was not entirely natural. Lemon, grapefruit, and orange were convincingly similar to the fruit found in nature. Watermelon, grape, and lime bore little resemblance to the actual fruit, but rather resembled the imaginary flavors found in soda and candy. The flavor, for example, was rich with the taste of lime. It was not at all like the lime that grows on trees; it was a perfect, rounded, floral taste of lime candy.










































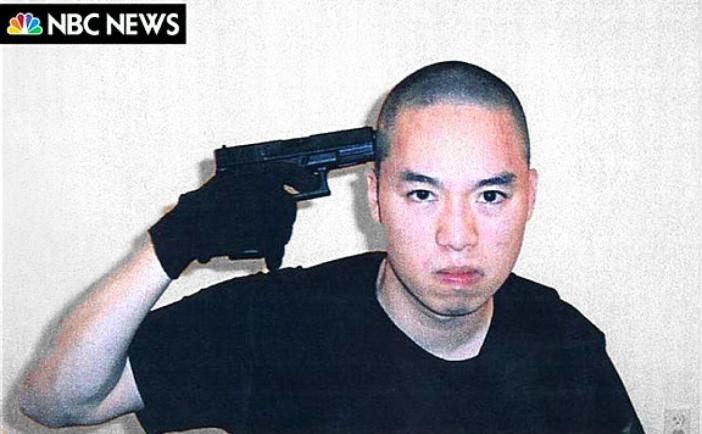 Seung-Hui Cho, who killed 32 and wounded 17 at Virginia Tech, Blacksburg, Virginia (Photo: NBC)
Seung-Hui Cho, who killed 32 and wounded 17 at Virginia Tech, Blacksburg, Virginia (Photo: NBC) Adam Lanza, who killed 20 students, six staff, and then his mother in Newtown, Connecticut
Adam Lanza, who killed 20 students, six staff, and then his mother in Newtown, Connecticut